Radiation Therapy
What to expect when going through Radiation Therapy
What is Radiation Therapy?
Radiation therapy, or radiotherapy, is the use of various forms of radiation to safely and effectively treat cancer and other diseases. Radiation Oncologists may use radiation to cure cancer, to control the growth of the cancer or to relieve symptoms, such as pain. Radiation therapy works by damaging cells. Normal cells are able to repair themselves, whereas cancer cells cannot. Radiation therapy can be given externally (External beam radiation therapy) where the radiation beam comes from a machine outside of your body at a precise point in your body. Radiation therapy can also be given from inside the body called Brachytherapy. Radiation therapy does not make you radioactive. It is safe to be with your family, friends, children and pregnant women while undergoing treatment.
The treatment team
Radiation therapy is prescribed by a specialist doctor called a Radiation Oncologist. The prescribed treatment is then planned by Radiation Therapists in conjunction with the Radiation Oncologist, and Radiation Therapists deliver the treatment. Medical Physicists assist and advise in aspects of the planning, treatment and quality assurance. Radiation Oncology Nurses assist with education, dressings, skin care and other medical needs during your treatment. There are also other allied heath staff that work in the cancer therapy centre (CTC) who you may see if required, such as Dietitians, Speech Therapists, Occupational Therapists, Social Workers and Clinical Psychologists.
This ‘Patient Pathway’ video from targeting cancer outlines the pathway that you as a patient will go through when being treated using radiotherapy.
‘Patient Pathway’ video link.
What you can expect
As every patient and treatment is different, the Radiation Oncologists and Radiation Therapists work together to determine how to best deliver the radiation therapy to you. Before you undergo radiation therapy, your healthcare team will guide you through the planning process to ensure the radiation reaches the precise point in your body. Planning includes:
Simulation:
During simulation, your radiation therapy team works with you to find a comfortable position for you during treatment. It's important that you lie still during treatment, so finding a comfortable position is vital. The Radiation Therapist will perform the CT simulation. They will:
- Get you to lie on the same type of bed during CT as will be used during treatment.
- Use cushions and other immobilisation devices to position you in the right way and to help you hold still.
- Make immobilisation devices for you, if needed. Patient’s receiving treatment to the head, neck or brain often have an immobilisation device made during simulation. You can access more information on mask making on the Head & Neck Cancer Australia website.
- Mark the area of your body that will receive the radiation. Depending on your situation, you may receive temporary marking with a marker or you may receive small permanent tattoos. Tattoos are small permanent marks on the skin, approximately the size of a freckle, which will help the Radiation Therapists to position you the same way every day during treatment.
- For some treatments you may be asked to hold your breath in order to reduce the area that will be treated, or to limit the radiation dose received by organs such as the heart. Your radiation oncologist will discuss this with you prior to simulation if they think this may be a suitable option for you. Explanations on deep inspiration breath hold (DIBH) and exhalation breath hold (EBH) can be seen in the videos on this page. If you are unable to do this, please do not worry.
Your radiation oncologist may recommend additional simulation imaging using MRI or PET. This will be discussed with you by the Radiation Oncologist before simulation.
CT simulation appointments generally take between 30-45minutes.
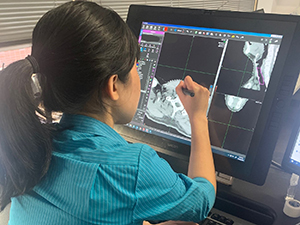
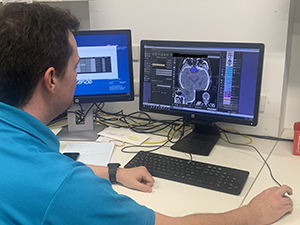
Planning:
Treatment planning is done by your radiation team after your CT simulation appointment. Using the information gathered from the simulation, your team works together behind the scenes to design your personalised treatment plan. This will generally take approximately 2 weeks.
Your treatment plan includes:
- The number and types of beams needed to treat the area
- The number of radiation treatments you will need
- The amount of radiation you will receive at each treatment appointment
Treatments plans are different for each person. Some treatment plans are given in only 1 day and others may be given over several weeks. On average, radiation treatments are given daily for 4 to 5 weeks.
Treatment:
The Radiation Therapists will position you on the treatment bed. Once you are positioned, the bed will be moved under the linear accelerator (the radiation machine). The Radiation Therapists will check measurements and take images to make sure you are in the right position each day.
The Radiation Therapists will not stay in the treatment room with you during treatment. They can see you through a camera while you are receiving treatment and will make sure you’re okay. There is an intercom in the room that you can use to speak to them whenever you need to.
The linear accelerator will not touch you during the treatment sessions. It may move around your body during the sessions to give you radiation from different angles.
Radiation treatment doesn’t hurt. You will not see or feel anything during the treatment. You may hear clicking or whirring noises from the machine. These noises are perfectly normal. Radiation treatment does not make you radioactive.
When the radiation treatment is finished, the Radiation Therapists will come back into the treatment room. They will remove any immobilization devices and help you off the bed. They will also be able to help you with any side affects you may be having.
Each radiation treatment room has a music player. You are welcome to choose your music to listen to while you have your treatment.
There are several different types of treatment delivery machines in the CTC.
- Linear Accelerators-
Most patients treated at the CTC will have their treatment on a linear accelerator. These machines produce high energy x-ray or electron radiation. You will not feel or see anything during treatment, but will hear the machine making a buzzing noise. The treatment is very similar to having an x-ray taken.
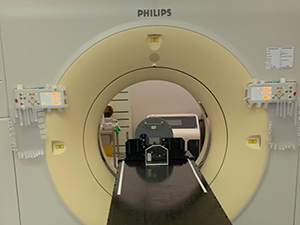
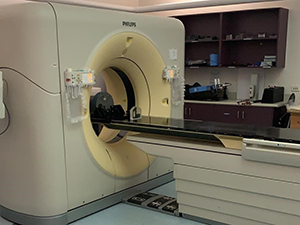
- Tomotherapy -
This machine looks like a CT scanner, but is also able to deliver radiation treatment. It is used for some head and neck treatments, and other complex cases.
- Superficial/Orthovoltage -
This machine is smaller than a linear accelerator and is used for superficial areas such as some skin cancers. The head of the machine comes very close to the area to be treated and in some cases will touch the skin.
- Brachytherapy -
Brachytherapy involves delivering the treatment using a small radioactive source that enters the body. The source is positioned by an applicator that is placed in body cavities or through needles placed in tissue. Sometimes a mould placed on the skin is also used. Brachytherapy can be given in conjunction with external beam radiation therapy or alone. You will not be radioactive after treatment.
 |
 |
Side Effects:
A variety of side effects may be experienced depending on the area of the body being treated and usually occur 1-2 weeks after the commencement of treatment. Every person will experience different side effects and most patients complete treatment without major problems. The radiation oncologist will explain possible side effects with each patient. Radiotherapy does not cause the patient to be radioactive.
General side effects include tiredness and red itchy skin in the treatment area. Tiredness occurs because it is part of your body’s natural healing process and because of the stresses placed on you as you attend radiation therapy department daily. The skin within the treatment area may become red and itchy, like sunburn, but this reaction can be lessened by avoiding soaps, creams, deodorants and talcum powder, as well as avoiding shaving or hair removal in the affected area. It is only necessary to avoid putting these products in the treatment area once treatment has begun. More information will be provided to you by the radiation oncology team during your appointments.
A list of useful resources on potential side effects for each treatment site can be found at the following links:
Targeting Cancer
EviQ
Head & Neck Cancer Australia
Cancer Council
Other Facilities:
There are many other services and facilities to assist patients undergoing treatment at the CTC. Some of the services are listed below. Please ask if you want more information.
Dietitian
Wig library
Social worker
Cancer group programs
Clinical Psychologist
Look Good, Feel Better
Occupational Therapist
Physiotherapist
Speech Pathologist
Resource Centre
Wellness Centre
Useful Resources:
Targeting Cancer
Cancer Council NSW
Head and Neck Cancer Australia
EviQ
Patient support group
RETURN
TO TOP
|